Genetic and environmental risk in dementia
 Although a small proportion of cases of dementia are caused directly by gene mutations, the majority of cases are sporadic with no known cause. However, there are a number of factors that can increase our risk of developing dementia, including both environmental and genetic factors. Although we have no control over some risk factors, such as ageing and our genetics, many lifestyle risk factors are modifiable. Understanding dementia risk factors, both environmental and genetic may result in opportunity to implement interventions to reduce the risk of dementia lower the burden of dementia as our population ages.
Although a small proportion of cases of dementia are caused directly by gene mutations, the majority of cases are sporadic with no known cause. However, there are a number of factors that can increase our risk of developing dementia, including both environmental and genetic factors. Although we have no control over some risk factors, such as ageing and our genetics, many lifestyle risk factors are modifiable. Understanding dementia risk factors, both environmental and genetic may result in opportunity to implement interventions to reduce the risk of dementia lower the burden of dementia as our population ages.
Current projects
iPSCs to understand genetic risk
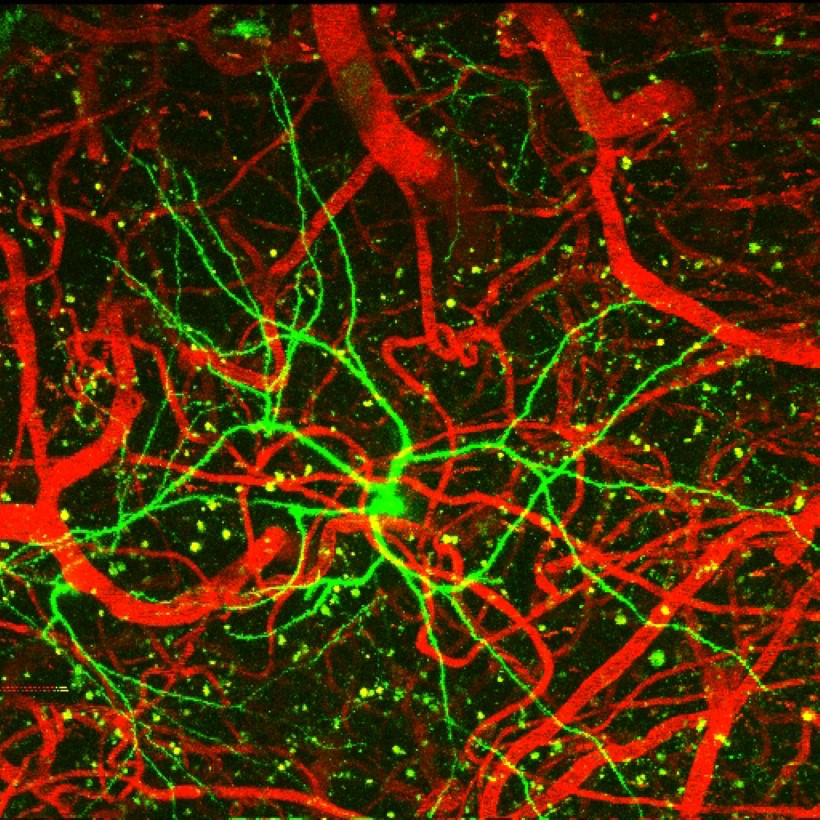
One limitation in neuroscience research is our inability to obtain neural tissue from living persons. To overcome this, we use molecular techniques to ‘re-program’ skin cells into stem cells, that we can then use to generate nerve cells in the laboratory. In this way, we are able to study tissue that correspond to persons with different disease-specific genetic risk factors or causative mutations, and to investigate how nerve cell function is changed because of these genetic changes. We also use sophisticated gene editing techniques that enable us to correct the genetic change in cells grown in the laboratory. When combined with our expertise in stem cell biology, gene editing will expedite the translation of genetic findings into clinical practice by providing unique, relevant and specific platforms for novel biomarker identification, or for drug discovery experiments that seek to promote neuron function.
- Objectives: To develop human cell-based models to understand genetic risk of brain and eye diseases
- Research Team: Dr Anthony Cook, Assoc Prof Anna King, Prof James Vickers, Dr Jana Kopecna
- Collaborators: Assoc Prof Alex Hewitt (Menzies Institute for Medical Research), Assoc Prof Alice Pébay (Centre for Eye Research Australia)
- Funding: Wicking Dementia Centre, University of Tasmania, Royal Hobart Hospital Research Foundation, Clifford Craig Foundation, ORIA
Epigenetics in AD
Alzheimer’s disease (AD) is a complex disease in which genetic and environmental risk factors interact and contribute to disease onset and progression. All of the cells in our body have the same DNA code, and in healthy individuals the right genes are expressed in the right amount, in the right cell types at the right time. This is achieved by the addition or removal of small chemical residues on top of the DNA (methylation), and modifications that alter how our DNA is packaged (histone modifications). Epigenetic marks on our DNA can change in disease and increasing evidence suggests that epigenetic changes contribute to the disease process in AD. However, few studies of epigenetic alterations in AD examine epigenetic changes in specific cell types (and the brain is made up of many different cell types) or assess the different epigenetic layers together (eg. DNA methylation and histone modifications). For example, we recently discovered that a subset of neurons (that are particularly susceptible to death in AD) contain DNA methylation marks outside of the nucleus that are reduced in human AD brains compared to healthy control brains.
- Objectives: To identify the key alterations across multiple epigenetic layers, including direct measurement of both histone modifications and DNA methylation, occurring in neurons in relevant transgenic AD rodent models and in human tissue.
- Research Team: Dr Phillippa Taberlay, Dr Adele Woodhouse, Prof James Vickers, Andrew Phipps (student).
- Collaborators: Prof Mark Robinson (University of Zurich); Dr Timothy Mercer (Garvan Institute of Medical Research)
- Funding: Judith Jan Mason and Harold Stannett Williams Memorial Foundation National Medical Program grant; Alzheimer’s Australia Dementia Research Foundation, Yulgilbar Foundation, Wicking Dementia Centre, University of Tasmania.
Traumatic brain injury and dementia
There is increasing evidence that traumatic brain injury may be a risk factor for the development of dementia with single or multiple injuries linked to the development of Alzheimer’s disease, chronic traumatic encephalopathy and other forms of dementia. Understanding the changes in the brain that result in the progress of pathology will aid in the development of guidelines for the treatment of brain injury and concussion. We are using both cell culture and animal models to examine the cellular and functional effects of brain injury on Alzheimer’s disease related pathology as well as the effect of the timing of injury.
- Objectives: To investigate the links between brain trauma and the pathological changes that lead to the development of dementia
- Research Team: Professor James Vickers, Associate Professor Anna King, Associate Professor Alison Canty, Dr Matthew Kirkcaldie, Dr Jenna Ziebell, Alex Cronk (student)
- Collaborators: Dr Nicole Bye
- Funding: Wicking Dementia Centre, University of Tasmania, ARC Discovery Grant DP140103094
Stress and dementia
There is a growing evidence that negative mental factors such as prolonged stress, depression and social isolation may increase risk of dementia. Relatedly, there appears also to be an interplay between AD pathology and the hypothalamic-pituitary-adrenal (HPA) axis, the neuroendocrine system responsible for regulating the body response to stress. Consistent with other studies, we have recently determined that a common familial mouse model of Alzheimer’s disease demonstrates elevated levels of the major rodent glucocorticoid stress hormone, corticosterone. Furthermore, once the HPA axis is affected, novel environments, which would normally be enriching, may become stressful and enhance Alzheimer’s disease pathology. We are using a multi-faceted approach from cell culture and animal models of Alzheimer’s disease, through to a human cohort study, to investigate the role of stress in dementia.
- Objectives: To investigate the role of stress in Alzheimer’s disease
- Research Team: Professor James Vickers, Associate Professor Anna King, Associate Professor Alison Canty, Dr Duncan Sinclair, Dr Matthew Kirkcaldie, Kim Stuart
- Collaborators
- Funding: Wicking Dementia Centre, University of Tasmania
Sleep and dementia
One of the most prominent features of Alzheimer’s disease is the presence of senile plaques in the brain, which are waxy aggregates of waste protein offcuts, thought to damage the connections and cells of the brain, leading to the symptoms of the disease. In recent years the importance of sleep in clearing waste materials from the brain has been the focus of considerable research, leading to the notion that disturbances of sleep might lead to increased waste accumulation, and possibly increase the rate of plaque growth. This agrees with the fact that in humans, both insomnia and sleep apnoea increase the odds of developing Alzheimer’s disease. Our studies use genetically modified mice which grow plaques in the brain, to examine whether moderate sleep disturbance over a period of several months will increase the amount of pathology in the brain.
- Objectives: To investigate the possible role of sleep disturbances on the pathology of Alzheimer’s disease
- Research Team: Dr Matthew Kirkcaldie, Assoc Prof Anna King, Prof James Vickers, Justin Dittmann, Ellie Bucher (student), John McManus, Aidan O’Mara (student)
- Collaborators
- Funding: Mason Medical Research Fund, Equity Trustees