| Home | Course Overview | Student Information |
| Assessment & Evaluation | Student Experience | Frequently Asked Questions |
The University of Tasmania Graduate Quality Statement sets out the attributes and qualities that graduates of the University will possess at the conclusion of their study:
The University of Tasmania experience unlocks the potential of individuals. Our graduates are equipped and inspired to shape and respond to the opportunities and challenges of the future as accomplished communicators, highly regarded professionals and culturally competent citizens in local, national, and global society. University of Tasmania graduates acquire subject and multidisciplinary knowledge and skills, and develop critical and creative literacies and skills of inquiry. Our graduates recognise and critically evaluate issues of social responsibility, ethical conduct and sustainability. Through respect for diversity and by working in collaborative ways, our graduates reflect the values of the University of Tasmania.
Medicine (BMedScMD) Program structure
The Medicine Program employs the Australian Medical Council Graduate Outcome Statements (AMC GOS) as the graduate outcomes for medical students and these align with the University Graduate Quality Statement.
The Medicine curriculum uses a learner-centred approach; specifically, it seeks to help students align their thinking in response to encounters with new information or situations. The teaching and learning strategies in the Medicine Program are designed to challenge students to explore their current concepts and develop new thinking.
Another important principle is that of 'situated' learning which encourages engagement and enhances recall. There is a focus on regular Case Based Learning (CBL) activities to aid integration and highlight important concepts.
Medicine program: teaching locations
The Foundation Years of the Medicine program are taught around Hobart at the University of Tasmania Medical Science Precinct and additional community locations.

The clinical years of the program are taught at a Clinical School. The Tasmanian School of Medicine has three Clinical Schools; the Hobart Clinical School, the Launceston Clinical School and the Rural Clinical School based in Burnie.
From 2025, the BMedScMD course will be offered in its entirety at both the Hobart and Cradle Coast (Burnie) campuses, using new Commonwealth grant funding to embed statewide training for medicine.



More information and key contacts for the Clinical Schools.
You can also take a “virtual” look at the Tasmanian School of Medicine Medical Sciences Precinct (MSP) to orient yourself to the MSP building with the online tour.
Student outcomes
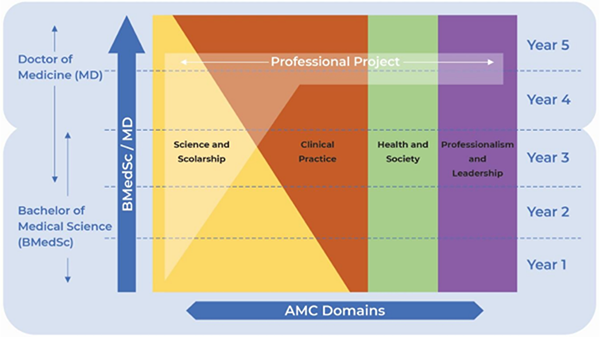
The Medicine program curriculum has four domains as an organising principle under which the learning outcomes are grouped and assessed. They incorporate the University of Tasmania's generic graduate statement outcomes and the AMC Graduate Outcome Statements (GOS) recommendations regarding knowledge, skills and attitudes of a medical graduate in Australia and New Zealand. Medical students graduating from the Medicine program will achieve the AMC GOS embedded in these four domains, which collectively provide the requirements that students must demonstrate at graduation. The early years of the program address fundamental system and diagnostic assessment skills, knowledge and professional behaviours, while integrated learning in the clinical years builds upon these foundations to synthesise and integrate students’ learning across the four domains. The Professional Practice Project allows students to complete a project in an area of interest that may sit in or across multiple Domains.
The four domains are:
- Clinical Practice: the medical graduate as practitioner
- Professionalism and Leadership: the medical graduate as a professional and leader
- Health and Society: the medical graduate as a health advocate
- Science and Scholarship: the medical graduate as scientist and scholar
The AMC Standards for Assessment and Accreditation of Primary Medical Programs contains extensive information on the domains, graduate outcomes and standards that universities have to meet to have an accredited medical course. The Medicine program must achieve accreditation by the AMC on a regular basis and provides annual reports about the course to the AMC.
The professional behaviours and ethics expected of medical practitioners and students are set out in Good medical practice: a code of conduct for doctors in Australia, published and reviewed regularly by the Medical Board of Australia. The Medicine program embeds opportunities for students to develop and enhance the knowledge, skills and attributes required for practice as a junior doctor in the curriculum.
It is important that the AMC Graduate Outcome Statements are interpreted according to the level of training and experience that will have been gained by an entry-level practitioner. When you graduate you will not possess the clinical experience, leadership skills or advocacy skills of an experienced practitioner. What you will have achieved is a foundation upon which you will be thoroughly prepared for internship, and from which you can build and develop your expertise in all fields of the profession.
Medical education is a continuum, and many of the outcomes specified will be reflected further in the outcomes expected from early postgraduate training and throughout your medical career, as you continue to develop your clinical abilities.
Orientation
All commencing students are required to attend course orientation and briefing sessions provided by Tasmanian School of Medicine academic staff in the first week of semester. These sessions contain a detailed overview of the curriculum and what students need to know about studying with the School. The Tasmanian Medical Students’ Society (TUMSS) also provides new students with opportunities to meet other medical students and lecturers, and to be taken on brief tours of the Medical School’s facilities.
Course learning outcomes
The curriculum aligns with the AMC Graduate Outcome Statements (GOS). The four domains of the AMC GOS provide a structural basis for managing the delivery and assessment of the program. However, learning is integrated across the domains and many learning and assessment activities will reflect this.
The ILOs of each unit are set out in the Unit Outline and you should pay close attention to this outline. In Year 4 and 5 the AMC GOS are used to structure learning. The ILO mapping is also available as a link in each MyLO section for BMedScMD units.
Delivery principles
The Medicine program curriculum uses a learner-centred approach focusing on Case Based Learning (CBL). CBL is described as active learning focused upon a clinical, community or scientific problem. In CBL tutorials, students consider a series of cases (clinical presentation or problems) relevant to the human body system under consideration and have related teaching throughout the week. These clinical cases provide a framework for students to learn normal structure and function, wellness and disease, clinical history and examination, analytical thinking, clinical problem solving and evidence based medicine. In addition, elements of community health and medical professionalism are incorporated into cases. CBL is facilitated by tutors with backgrounds as clinicians, general practitioners, and academics in health science related fields.
In addition to CBL the modes of learning and teaching in the Medicine program include keynote sessions, small group tutorials, practical and clinical skills sessions, seminars, workshops, online activities, student-led presentations, self-directed learning activities and learning within clinical placements. Self-directed learning throughout the program is designed to foster a positive approach to life-long learning
Special Programs
- Anatomy Program
The Tasmanian School of Medicine has a highly regarded anatomy program that employs dissection as a learning methodology, as well as advanced imaging and laboratory work. Students have one of the best opportunities in Australia to engage with the human body and this program is integrated with units from the commencement of the BMedScMD.
- Kids and Families Program (KFP)
This program runs from the middle of first year until the middle of third year. KFP aims to allow students to develop understanding of child growth, development and behaviour, common childhood illnesses, and the role of the family and preventive health. KFP incorporates consideration of the determinants of family health, developing professionalism and communication skills. In first year, small groups of students are introduced to a volunteer family that are about to have (or have just had) a baby, and visit the family on a regular basis over the next two years. Students report on these visits and discuss their experience with other students and tutors. KFP contributes to the overall assessment of the units of learning in these years.
- Clinical Skills Program
In first and second year the opportunity for learning in clinical settings is afforded through a series of short community visits and clinical placements. In third year, students undertake longer and immersive clinical placements within the hospital or community
In Years 3-5, the course runs in the three Clinical Schools: the Hobart Clinical School (HCS), Launceston Clinical School (LCS) and the Rural Clinical School (RCS) in Burnie. In Years 4-5, students spend the majority of their time in clinical settings where there is continued emphasis on clinical practice and applying knowledge of all material previously covered in the program.
All students are expected to attend Orientation at their individual Clinical Schools. The Orientation schedule will be made available to all students in January of their year of study.
The clinical skills that students are expected to learn in the Medicine program can be recorded in the student logbook across all years of the BMedScMD and practiced in the clinical skills, Patient Partner, and Kids and Families programs, and during clinical placements.
Self-directed learning and extracurricular activities
Students in the Medicine program are expected to engage with opportunities that complement the curriculum. These activities can be set out as part of a student’s learning portfolio and can contribute to the narrative of your learning in the years you spend at the Tasmanian School of Medicine. This type of learning can also help you decide where to focus your personal and career aspirations.