CAA108 - Principles of Paramedic Practice 2
Allan Ajifo
right brain

This work is licensed under a
Creative Commons Attribution 2.0 Generic License.
Hide image information
Lisa Bowernan
Janelle White
Neurological Disorders
Slide 1: A & P Review
This image is licensed under the Creative Commons Attribution 3.0 Unported license: Attributed to OpenStax College via wikimedia commons
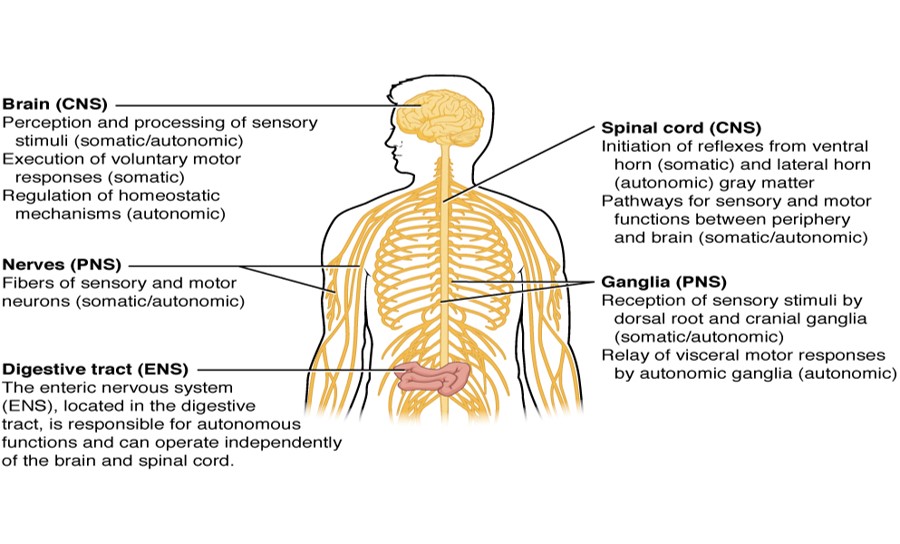
- Basic Functions of NS
- NS – 2 divisions…
- CNS…
- Brain…
- Blood supply…
- BBB…
- RAS…
- Spinal cord…
- PNS…
Slide 2
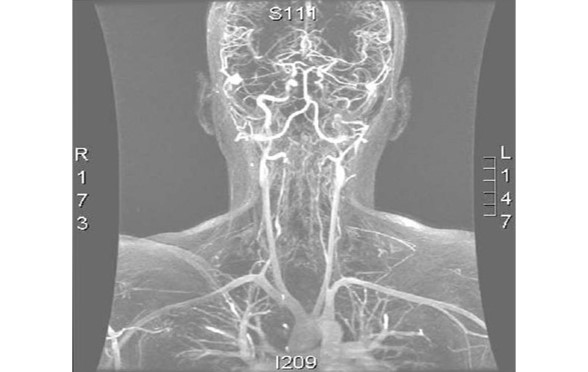
"Angio MR" by Germain Orphanet Journal of Rare Diseases 2007 2:32 doi:10.1186/1750-1172-2-32. Licensed under CC BY 2.0 via Wikimedia Commons
Arteries and veins of the brain. Wellcome Library, London [CC BY 4.0], via Wikimedia Commons
This work is in the Public Domain.
Attribution: Rhcastilhos (Gray519.png) [Public domain],
Sourced via Wikimedia Commons
Slide 3: Altered Mental State (AMS)
"Confusion" is licensed under the Creative Commons Attribution-NonCommercial-NoDevivs 2.0 license: Attributed to Smythe Richbourg
- Definition?
- How do we determine if our patient has an AMS?
- What tools do we have to use?
Slide 4: Concussion
Fully reversible brain injury that does not involve any bruising or structural damage to the brain.
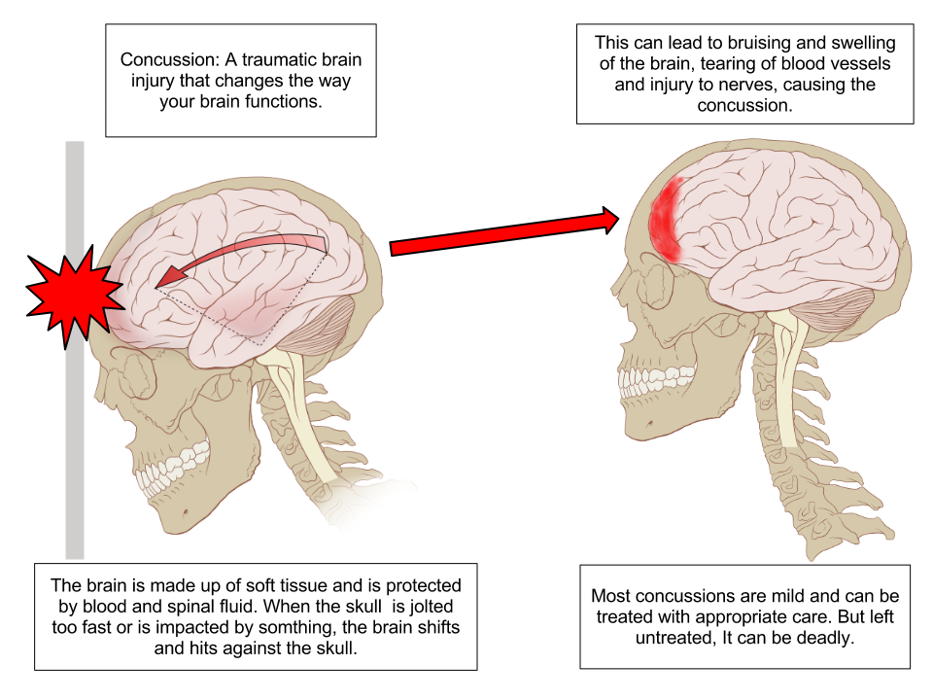
"Concussion Anatomy" is licensed under the Creative Commons Attribution-Share Alike 3.0 license: Attributed to Max Andrews via Wikimedia Commons
Slide 5:

Utah cowboy (explored) is licensed under the Creative Commons Attribution-NonCommercial 2.0 Unported license: Attributed to Elizabeth Haslam
- Mild to moderate impact to skull
- Brief LOC (< 5 min)
- Temporary disturbance of function
- ? Mild Retrograde amnesia
- Drowsiness, irritability, confusion.
- True concussion – does not get worse!
- A lucid interval = a temporary improvement in a patient's condition after a TBI, after which the condition deteriorates, sometimes rapidly.
- A lucid interval is especially indicative of an epidural haematoma.
- An estimated 20 to 50% of patients with epidural haematoma experience a lucid interval
Retrograde Amnesia: No memory of what happened just before an event
Anterograde Amnesia (for interest only): inability to create new memories post event
Slide 6: Unconsciousness: the ultimate AMS
Acid Queen is licensed under the Creative Commons Attribution 2.0 license: Attributed to Ian Burt
Definition…
“What’s blood got to do, got to do with it!”
4 Broad Causes:
- Blood oxygenation problems?
- Blood circulation problems?
- Metabolic problems?
- CNS problems?
May be a combination, such as?
Slide 7: The Greedy Brain

This image adapted from 24k Jumping Brain is licensed under the Creative Commons Attribution-NonCommercial 2.0 license: Attributed to Emillio Garcia
- The brain represents only 2% of body weight
- It receives 15% of the cardiac output
- Uses 20% of total body oxygen consumption and
- Uses 25% of total body glucose.
Slide 8
A – Alcohol?
E – Epilepsy?
I – Insulin?
O – Overdose/Oxygen?
U – Underdose/Uraemia?
T – Trauma/Temperature?
I – Infection?
P – Poisoning/Psychosis?
S – Stroke/Shock/Structural?
Slide 9: Scenario #1
C/T 79 year old male - collapsed. Thoughts?
Upon arrival you are greeted at the door by an anxious wife stating that she cannot wake her husband.
You walk to the back bedroom and find an elderly man lying in bed. As you enter the room, you can hear his gurgling respirations.
What are your initial actions?
Slide 10: Primary Survey
No detectable ‘dangers’
Response – patient opens his eyes to your voice. Unable to communicate or speak.
A – airway
B – breathing
C – circulation
D – disability /dysfunction
E – exposure/environment
F – focused history & adjuncts
Slide 11: Secondary Survey
Designed to identify & rectify other injuries/illness not identified in the primary survey.
- Head to toe examination - ask and you shall find!
- Take the history (from relative)
- What questions will you ask?
- Reassess what?
- Do you have an DDx and illness script in mind?
Slide 12: S & S

Myasthenia is licensed under the Creative Commons Attribution- Share Alike 3.0Unported license: Attributed to Cumulus
Managing the business
F.A.S.T
Decreased LOC
Unequal pupils
Facial droop
Inability to speak
Paralysis (hemiplegia)
Loss of bladder control (incontinence)
Other S&S not necessarily presented in this case…….
Slide 13: Pathophysiology of CVA or ‘Brain Attack’
Caused by an interruption of blood supply to the brain
- Atherosclerosis is usually a contributing factor to clot formation & narrowing of cerebral arteries
- Blockage Ischaemic Stroke
- Rupture Haemorrhagic Stroke
Stroke - 'The Window'
Medicine wants to call it Brain Attack now like heart attack to try and get people to understand the urgency – Time is Tissue and the fact that there is a window of opportunity usually 3-6 hours from onset of symptoms to act, and have thrombolysis or clamping of a bleed and possibly restore brain function.
Slide 14: Ischaemic Stroke (around 80%)
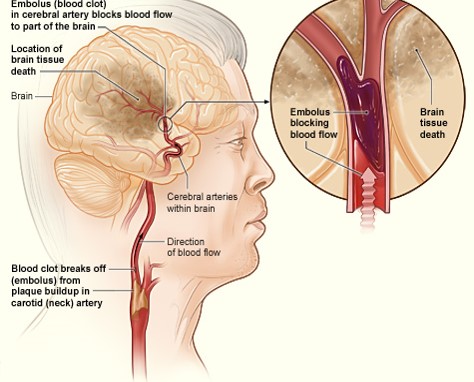
Ischemic Stroke By National Heart Lung and Blood Institute (NIH) (National Heart Lung and Blood Institute (NIH)) [Public domain], via Wikimedia Commons.
Cerebral artery is blocked by a clot or other foreign matter
- Thrombotic stroke (most common type)
- The narrowing and eventual occultion often occurs over a long period of time - S&S much slower,
- Headache not commn
- Embolic stroke
- Usually originates from the carotid artery or the heart (AF) - clot travels unit it lodges in a small cerebral artery blocking blood flow.
- Onset of S&S more sudden - headache, seizure activity or brief periods of unresponsiveness are more common
Slide 15: Haemorrhagic Stroke
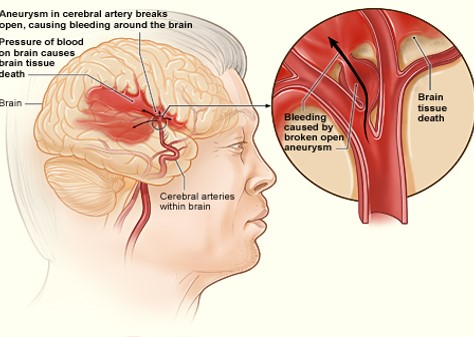
Haemorrhagic Stroke By National Heart Lung and Blood Institute (NIH) (National Heart Lung and Blood Institute (NIH)) [Public domain], via Wikimedia Commons.
- Rupture of an artery causing bleeding within the brain ICH or in the space around the outer surface of the brain SAH
- Often associated with hypertension
- Subarachnoid (SAH) often associated with aneurysms
- SAH commonly due to trauma
Slide 16
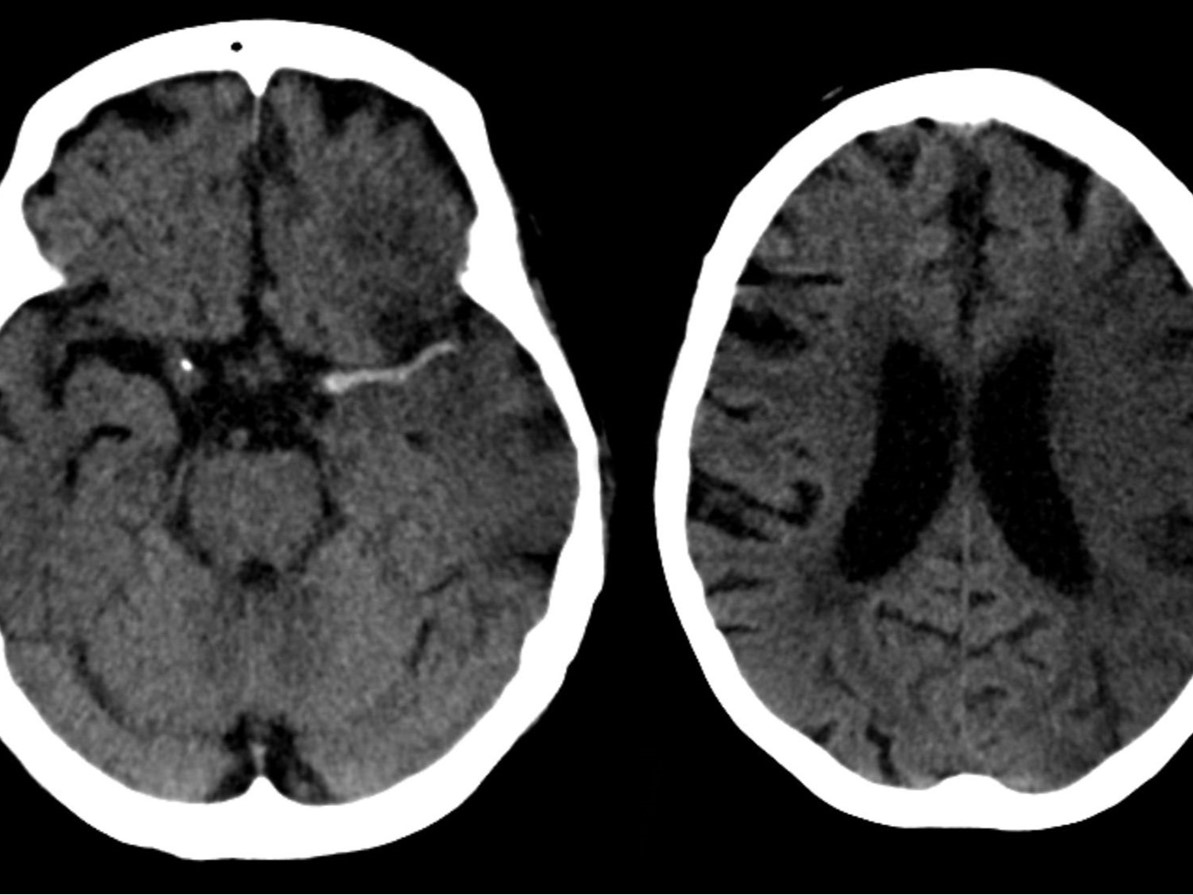
Left image: Haemorrhage.
Right image: Ischaemia.
This image is licensed under the Creative Commons Attribution- Share Alike 3.0 Unported license: Attributed to Hellerhoff via Wikimedia commons
Slide 17: Differentiating CVAs
-
Can only be done in hospital…
-
Hospital diagnosis essential to treat correctly…
- Ischaemic stroke fibrinolytics (clot busters)
- What would happen if you gave this to a patient suffering form a haemorrhagic stroke?
3 things we must do are:
-
Recognise, Notify, Transport!
Slide 18: CVA Vs TIA
- What is a TIA?
- CVA Vs TIA?
- How to treat CVA/TIA?
- Usually very frightening for the patient and family
- Primary & secondary survey as usual
- Reassurance +++
- Reassess
- Supplement with O2 only if Sats <95% - Why?
Slide19: Scenario #2
You are called to a 32 year old female complaining of severe headache in an ‘office’ in the CBD.
-
What provisional diagnoses are going through your mind as you drive to the address?
Slide 20: DRABCDE – Primary Survey
The patient is lying down on a couch. When you approach her, she opens her eyes and states…
“Thank goodness you’re here, I can’t take this pain anymore”.
While doing your primary survey. What questions do you want to ask?
Slide 21:
Primary Headache Disorders
- Can have vascular, muscular, and nerve aetiologies
3 Main Primary
- Migraine
- TTH
- Cluster
According to the WHO 35 types! Within the Primary and Secondary categories.
Slide 22: Your Community Pharmacy Assessment Task
MIGRAINE
International Headache Society criteria:
Should have 2 from column A and 1 from column B
Column A |
Column B |
One-sided headache |
Nausea and Vomiting |
Throbbing |
Sensitivity to light and sound |
Moderate - Severe and restricts function |
|
Worsened by activity |
Slide 23 : TTH
This image is licensed under the Creative Commons Attribution -Share Alike 3.0 Unported license: Attributed to Kevjonesin via wikimedia commons
(Tension Type Headache)
The most common!
Slide 24: Serious Causes of Headaches

This image is in the public domain
-
Brain tumour
-
SAH
-
ICH
-
Meningitis
-
Hypertension
-
Hypoglycaemia
-
CO poisoning, other toxic inhalation
-
Fever
-
Hypoxaemia
-
Stroke
-
Depression
Slide 25: Headache Symptoms to Take Seriously
- Persistent headaches that progressively worsen over days or weeks
- Headaches that start suddenly (especially important if never had them before and over 50 years old)
- Headaches that come on suddenly after coughing, straining, or exertion
- Changes in vision, double vision, increased weakness, or loss of sensation
- Confusion or changes in memory, personality, or behaviour
- General weakness, numbness or slurred speech
- A stiff neck with a fever or a rash, or a seizure
- An unexplained fever or breathing problems (i.e. shortness of breath), which accompany the headache
- A sudden or dramatic change in the severity of your headaches
- Headache after a head injury or accident, or after a sore throat or respiratory infection
- A constant headache with no relief
- Persistent or severe vomiting
- Experiencing three or more headaches a week
- Use of a pain reliever every day or almost daily to relieve headache symptoms
- A very sudden and excruciating headache unlike any ever before
Slide 26: Management
-
Symptomatic treatment – PAIN relief!?
Options… -
Position of comfort – lights/noise
-
Beware pt. deterioration.
-
Consider (warning signs/serious causes)
-
REASSESS!
-
Which observations will be particularly important?
Slide 27: Scenario # 3

![Creative Commons Licence [Some Rights Reserved]](http://creativecommons.org/images/public/somerights20.gif) © Copyright Peter Jeffery and
licensed for reuse under this Creative Commons Licence.
© Copyright Peter Jeffery and
licensed for reuse under this Creative Commons Licence.
- You are called to the local cricket ground to a 29 year old male pt having a ?seizure
- You find your pt lying on his side?
- As approach you note there are no dangers
Slide 28: Primary Survey reveals….

Adapted from Think by Sam Howzit licensed under a Creative Commons Attribution 3.0 Unported License.
-
Pt unresponsive to verbal stimuli
-
Pt withdraws from painful stimuli
-
RR – 14 & deep, note loud snoring
-
Pulse - 112
-
Skin pink, warm, moist
Bystanders provide the following information
“One minute he was playing cricket when all of a sudden he collapsed to the ground and began shaking all over”.
Slide 29: Secondary Survey
You begin your head to toe assessment…
-
NAD
-
Pupils – PEARL (slightly dilated…why?)
-
Patient starts to stir, moving all limbs, looking about. Seems dazed.
-
What do you do now?
Slide 30 : Five minutes later …
-
Pt now alert and oriented.
-
Pt states he has was diagnosed with epilepsy 10 years ago.
-
Normally takes Tegretol and Epilim but ran out of Epilim 2 days ago.
–Thoughts so far??
-
While talking he begins to have another seizure…
-
What do you do now?
Slide 31: Back to our patient who is seizing…
ABC’s of Seizure Treatment:
| A – AIRWAY | *Arrange protection/remove dangers? |
| B – BREATHING | *Be prepared to give medication? |
| C – CIRCULATION | *Consider/treat associated conditions? |
| D – DISABILITY | *Determine patient disposition? |
| E – EXPOSE | *Epileptic or not? |
Slide 32
- Approximately 1 in 120 people have epilepsy and up to 5% of the world’s population may have a seizure at some time in their lives.
- Anyone can be affected by seizures at any age, most frequently diagnosed in infancy, childhood, adolescence and old age.
- Epilepsy is diagnosed when the seizures are unprovoked and recurrent – in other words they happen more than once.
- It is estimated that around 50 million people in the world have epilepsy at any one time. Incidence in developing countries is almost double that of developed countries.
- Approximately 70% of people who have epilepsy surgery become seizure free.
- Treatment options for people who cannot get seizure control with medications include Vagus Nerve Stimulation and the Ketogenic Diet.
- Epilepsy is a condition of the brain, not a mental illness.
- People with epilepsy can obtain a driver’s licence if their seizures are controlled by medication or if they fulfil the guidelines set out by the driving authorities.
- There are around 40 different types of epilepsy and epilepsy syndromes and is not necessarily a lifelong disorder.
- Epilepsy is associated with an increased risk of death. (SUDEP)
Slide 33: The A-Z of other causes of seizures
Hippocampus:
- Abnormal levels of sodium or glucose in the blood
- Brain infection, meningitis
- Brain/Head injury
- Brain tumour (rare)
- Drug abuse
- Eclampsia
- Electric shock
- Fever (particularly in young children)
- Heat stroke
- Idiopathic seizures
- Illicit drugs, such as angel dust (PCP), cocaine, amphetamines
- Kidney or liver failure
- Phenylketonuria (PKU), which can cause seizures in infants
- Poisoning
- Stroke
- Very high blood pressure (malignant hypertension)
- Venomous bites and stings (see snake bite)
- Withdrawal from alcohol
- Withdrawal from certain drugs, some painkillers, benzodiazepines, valium
Slide 34: Medical emergency
“Status Epilepticus (SE)”
CSE, NCSE & RSE
- CSE = Convulsive seizure that lasts for > 5 minutes or 2 or more consecutive seizures without return of consciousness between (More critical)
- NCSE = Non-convulsive change in mental state from baseline for >30 minutes evidenced on EEG
- RSE = Refractory seizure activity that continues post antiepileptic drug therapy – considered when continued AMS
Slide 35: A note about Febrile Seizure
-
Caused by sudden high fever often >39°C
-
Most common in children 6 months to 6 years
-
5% of febrile children will have seizure
-
Secondary Seizure
-
Often short and may not require emergency care
-
Reassurance is essential
-
Does not mean child is or will become an epileptic
-
- These seizures will be covered in Paediatric subject next year.
Slide 36: Scenario # 4

This image is licensed under the Creative Commons Attribution-ShareAlike 2.0 Unported license: Attributed to William Murphy
It's a hot summers day at 1500hrs, when you are called to a person collapsed at the local RSL.
- What provisional diagnosis is going through your mind?
- What do you do when you arrive on scene?
Slide 37: Primary Survey

This image is in the public domain
- Nil Danger noted
- Responds to verbal command- however seems a little vague
- Responds appropriately when you ask who and where she is.
- RR – 22 regular, nil dyspnoea
- Weak radial pulse 102, regular
- Skin cool, moist, pale.
- TESTS?
- THOUGHTS?
- QUESTIONS?
Slide 38
Pt states she got up to go to the toilet and the next thing she remembers is everyone standing around her…
- Never happened before.
- Medications – Metroprolol & Lasix (furosemide)
- Nil allergies
- Played bowls all morning.
- Too hot to eat much lunch.
DIAGNOSIS??
THOUGHTS??
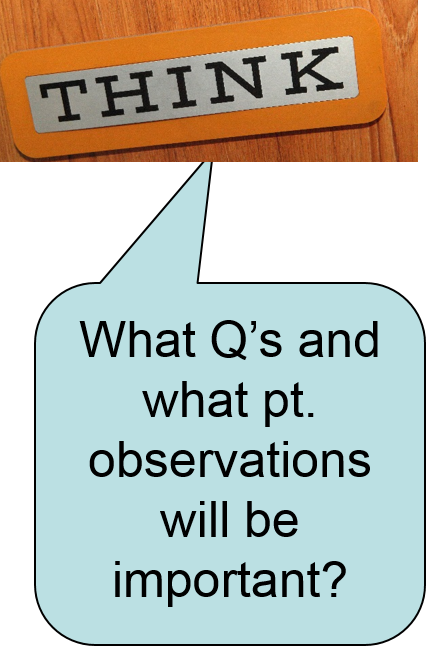
Slide 39: Syncope
-
aka ‘Fainting’
-
Sudden & temporary loss of consciousness.
-
Temporary lack of blood flow to the brain and the brain is deprived of 02 for a brief period.
-
Peripheral Nervous System frequently to blame
Slide 40: S&S of Syncope
-
Anyone experienced a syncopal episode?
-
How would you or the patient describe it?
-
Dropping like flies...
What are the differences between a Seizure & Syncope?
-
Syncope- pt usually standing
-
Syncope- pt remembers feeling faint or light-headed
-
Pt becomes responsive almost immediately after becoming supine
-
The skin is usually pale & moist
Slide 41: Assume the Worst
Use your clinical decision making skills… if something does not ‘seem right’ assume the worst …
What are other serious causes of syncope?
Slide 42: Syncope algorithm
Slide 43: Drugs & Syncope
Associated with LQTS & V-Arrythmias: (Antiarrhythmic, gastric motility promoters, Antibiotics) quinidine, sotalol, amiodarone, procainamide, erythromycin, haloperidol, tricyclic antidepressants.
Associated with Bradycardia: (Beta-blockers, Na channel blockers) verapamil, dilatiazem, digoxin.
Associated with Postural Hypotension: (Anti-hypertensive drugs, anti-Parkinson and diuretics) prazosin, Ca channel blockers, furosemide, nitrates.

This image is in the public domain
7 common Prodromal S & S
- Diaphoresis
- Pallor
- Nausea
- Palpitations
- Visual disturbance
- Hearing disturbance
- Dizziness
Slide 44: The Syncope Mnemonic
P – Pressure (vasovagal, orthostatic)
A – Arrhythmias (brady, tachy, blocks)
S – Seizure
S – ‘Sugar’ (hypo/hyperglycaemia)
O – Output (cardiac/oxygen)
U – Unusual (anxiety/hyperventilation)
T – Transient Ischaemic Attack/CVA)
Slide 45: What have we covered…
This image is licensed under the Creative Commons Attribution 2.0 license: Attributed to SOCIALisBETTER
- Review Neurological A & P
- Pathophysiology
- AMS
- Unconsciousness
- Common neurological conditions
- CVA/TIA
- Headache
- Seizures
- Syncope
Slide 46: Pick a card and focus on it for 3 seconds
The next slide will have removed your chosen card
Click here to see the next slideExcept where otherwise noted, content on this page is licensed under a Creative Commons Attribution-ShareAlike 4.0 International Licence
Note: The open version of this document may have been altered from the original. Only pages on this site that display the CC licence and logo are licensed under a Creative Commons licence.
| Attribution information | |
|---|---|
| Title: | Lecture Slides: 'CAA108' - Open Version |
| Source: | https://www.utas.edu.au/health/resources/open-resources/resources/courses/paramedicine/caa108-lecture-slides |
| Author: | Dr Lisa Bowerman |